There was a time when the disease was considered "age-related", but lately more and more often diagnosed "osteochondrosis" up to 35 years. This is due to a change in the pace of life - more people are involved in work sitting and sitting. And most importantly, physical activity, flexibility is reduced and, accordingly, blood circulation is impaired, which is the main thing in nourishing and restoring the spinal discs.
An interesting fact: according to statistics, more than 80% of the population, after 30 years, have changes in the spine, to a greater or lesser extent.
Reasons
Osteochondrosis is the general name for spinal aging. The process is directly related to changes in the structure of the vertebrae and discs. Under the influence of internal and external factors, disk thinning occurs. Appear - extensions, hernias, vertebral instability, changes in bone tissue, the appearance of osteophytes (thorns, growths). And all of these phenomena are complications of osteochondrosis. The course is chronic and without the lack of complex therapy makes it very difficult for further normal life.
You are probably familiar with the factors that provoke dystrophic changes, but we note again:
- Hypodynamics - contributes to the disruption of blood circulation in the neck, weakening of the muscle corset. Spinal curvature (flexion, lordosis, kyphosis, scoliosis).
- Long stay in a static position, and vice versa - increased loads and lifting weights.
- Injuries.
- Overweight, pregnancy.
- Heredity, metabolic disorders.
Man is the only creature on the planet suffering from spinal problems in the cervical spine. This is due to our ability to walk fully on foot, as well as muscle weakness and great neck mobility.
An important role in the formation of cervical osteochondrosis has a hereditary predisposition. Furthermore, it is not necessary for relatives to have osteochondrosis. The risk area includes people with a family history of degenerative and dystrophic diseases of the osteoarticular system (osteoarthritis, spondylitis, hernia, etc. ).
The neck is an important link. Many vessels and nerves pass through it to the brain. Problems in this part of the body will certainly affect the blood circulation in the brain and the work of the upper part - shoulders, arms. Degeneration develops gradually, with an increase.
Stages of development of cervical osteochondrosisIn the first stage, there is a local pain syndrome, accompanied by a sharp tension in the muscles, which increases the already unpleasant sensations, restricts movement.
Pain is expressed in 2 forms:
- Cervicago - "neck lumbago", a sharp sharp pain that appears when moving.
- Cervicalgia - attractive, painful, with constant muscle tension. It can take more than two weeks, even with proper treatment.
In the second stage, "radicular" syndrome is added - compression of nerves due to thinning of ligaments and discs. The pain appears when sneezing, coughing. If the patient is placed on his back and passively moves his head, then painful sensations will appear.
Numbness of the hand from the neck to the fingertips is characteristic, especially after sleep. The symptoms disappear quickly after active movements or placing the hand behind the head. If numbness or pain persists, complications (prolongation, hernia) may be forming.
There may also be a feeling of "freezing" of the shoulder with the onset of "arm-to-arm" syndrome - when arthritis of the shoulders and hands begins due to circulatory disorders in osteochondrosis.
Main symptoms
The main symptoms of cervical spine osteochondrosis include:
- Headache and dizziness.
- Localized pain, as well as possible radiation to the shoulder, occiput or shoulder (especially adhesion of the cervicothoracic region).
- Numbness and weakness in the hands.
- Lump in the throat.
- Hypertension (persistently high blood pressure).
- Decreased hearing and visual acuity, tinnitus (development of vertebral artery syndrome).
Interesting: changes in the disease affect important vessels in the neck that supply blood to the brain. In patients with chondrosis, there may be a "Sistine Chapel" syndrome - fainting after a sharp blow to the head.
Pain and its localization are often disguised as a serious disease - angina pectoris.
Diagnosis and treatment
is very important to treat the symptoms of cervical osteochondrosis at the beginning of degenerative processes. To do this, you should seek immediate help from a neurologist or vertebrologist. But practice shows that they seek help, already with complications - elongation, hernia, instability of vertebral bodies.
The patient should be thoroughly examined - ultrasound of the heart, blood vessels of the brain and neck, ECG, collection of urine and blood tests. Necessary weight to make an X-ray, and in some projections and in a stack with an open mouth (to see the beads that cover the teeth).
Unfortunately, doctors diagnosed with osteochondrosis regulate many diseases, as there is no time, experience, desire to identify the cause of this or that symptom. Treatments a treatment is prescribed that brings temporary relief, but the real cause remains undiscovered, over time everything comes back or brings no relief at all. This is the situation that makes people self-medicate.
Treatment of cervical spine osteochondrosis
Therapy should be as complete as possible.
- Physiotherapy.
- Drug therapy.
- Massage.
- Physiotherapy.
- Stretches.
- Stretching of the cervical spine according to Shishon's method.
- Abandoning customs.
Physiotherapy
The effectiveness of treating osteochondrosis of the cervical spine with the help of physiotherapy and therapeutic baths has been scientifically proven.
- They relieve pain syndrome.
- Elimination of inflammation.
- Increase the effectiveness of drug therapy and other methods of treating cervical osteochondrosis.
The therapeutic effect of physiotherapy in the form of low-frequency pulsed electromagnetic therapy in combination with radon baths, sometimes with iodine-bromine baths, increases.
Drug therapy
When complications of osteochondrosis occur in the cervical spine, hernia or large extensions, inflammation of the compressed nerve roots. Therefore, to relieve inflammatory symptoms and stop the pain, you need to pierce the course of intramuscular injections of vitamins - B1, B6, B12. Also, with impaired blood circulation, blood viscosity increases, which disrupts the blood supply to the brain with oxygen. It is necessary to take antiplatelet agents.
Drug therapy.
- Eliminates pain and inflammation.
- Accelerates metabolism in tissues that are disrupted due to impaired blood supply.
- Thins the blood, improving blood circulation.
Massage
The neck massage course is necessarily included in the treatment program for neck osteochondrosis.
- Muscle tension is relieved, thus releasing the constricted arteries located nearby.
- Improves blood circulation and tissue nutrition, which have a positive effect on the heart and brain.
- Muscle pain is reduced.
Unfortunately, good massage is not free and many reject this procedure because of the high prices. But in the medical complex, cervical spine massage should be included for the good of the issue. Even if they advise that it is not as necessary as physiotherapy exercises.
Physiotherapy exercises
Treatment of osteochondrosis with physical therapy of the cervical spine is the main method, without which cure is impossible. No pill can cure osteochondrosis without exercise therapy. Tune in to the fact that you have to do gymnastics every day for a whole year in order to permanently forget the symptoms of the disease.
Important: Exercise therapy is a 70% victory over osteochondrosis. Even if the pain disappeared, the disease is nowhere to be found. You can not relax.
Goals and objectives of exercise therapy.
- Strengthen the deep neck muscles and muscular corsets of the shoulder region, so that the muscles hold the head in the right position, without stress on the intervertebral discs, and no extensions are formed that squeeze the nerve endings. To enlarge the intervertebral space, thus eliminating the oppression of nerve roots.
- Bring painless movement while developing flexibility and mobility.
- Exercise speeds up and increases blood circulation, thus improving the nutrition of the intervertebral discs and surrounding muscles.
Important: Train yourself to do a series of exercises 3 times a day for the first 4 weeks, then 1 time a day for a year.
Neck Exercises
Before doing any exercise, you need to warm up your muscles.
Heating
We warm up the chest muscles and the cervical spine. Slow circular movements with the shoulders - front and back. Each muscle should work as hard as possible.

Circular shoulder movements - get up as much as possible, move back, down and then forward. When pulling back - join the shoulder blades together. And the same circles with each shoulder in turn.
Add the arms - and repeat the movements with the arms bent at the elbows. One by one, we will again join the shoulder blades as we get our hands back. And then we will also move our shoulders as much as possible.
This completes the heating. Let’s start by doing some basic neck exercises.
Exercise technique
Do all the movements slowly, so as not to injure yourself and prevent nerve entrapment.
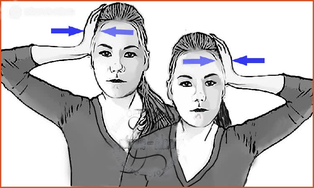
Get correct behavior. The shoulders are lowered, slightly set back, the chin is parallel to the floor. Static exercises are aimed at training the deep neck muscles. Each movement holds the resistance for 5-8 seconds. Release for two seconds and repeat again. So 5 times.
- We press the palm on the temple and press it trying to make the head, we resist with our head, preventing the hand from tilting the head to the side. Do the same on the other side.
- Put your hands on the lock, support your chin and press the resisting head.
- We resist with the forehead.
- From the back of the head
- Otherwise the head resists on the cheekbones
Along with strengthening the neck muscles, it is necessary to simultaneously strengthen the shoulder girdle. Some exercises with an extender should be included in the treatment complex 2-3 times a week.
Extra load
Exercise in the form of running, brisk walking, swimming, gymnastics will improve the overall blood circulation in the body. Especially from poor blood supply, the brain suffers, which needs oxygen for cervical spine problems. Exercises last at least 20-30 minutes, up to 2 times a week.
Dry pull of the cervical spine
The dry layout method is horizontal and vertical. This method is called traction - a very effective treatment for spinal osteochondrosis. Young people are easily fit for full recovery, using only one pull during treatment. Since disc recovery in youth is much faster. Of course, age impedes recovery and the ability to repair cartilage tissue, but traction still remains an important point in the complex treatment of neck osteochondrosis.
Alignment problems
- Increase the lumen between the vertebrae.
- Eliminate pain due to compression of nerve roots.
This procedure has contraindications, so do not do it without consulting your doctor. Previously, this method was practiced only in hospitals, sanatoriums and rehabilitation centers.

Stretching technique is now available at home using a treatment collar. The pull-up session lasts 15 minutes a day.
We have analyzed the entire treatment program for cervical spine, it remains to talk about the usual way of life, which also needs to change perfectly.
Important: all of the above methods should be discussed with your doctor.
Leaving habits
We understand that laziness and excuses lead to early osteochondrosis. If you do not get over them, then you do not need this article. Drink pain relievers and continue to live as before. Although you can try to fix some bad habits.
- Sleep on an orthopedic pillow and mattress.
- Do not lie on a high pillow for hours when your head is up while reading while playing on the phone. At this point, the cervical vertebrae compress the blood vessels, disrupting blood circulation.
- A stationary position on the computer when there is no control over time. Set your alarm clock every hour to warm up your stiff neck muscles.
- Move more - sports games, outdoor activities, walk 10, 000 steps a day.
Summary
Course procedures - injections, massage and physiotherapy are done 1 month every six months. During this period, physiotherapy exercises increase up to 3 times a day.
In other months every day:
- Exercise therapy - 1 time per day.
- Stretches.
Repeat the procedures after 5 months. And this rate is at least a year. Positive results are noticed within a month.
The above technique is not an algorithm for all cases of treatment of cervical osteochondrosis. All points should be discussed with a physician. But if the doctor prescribes only one method, for example physiotherapy, massage, then the effect will be temporary. The treatment is long, so it is best to immediately adjust to the success of the recovery. Trust me, you will not go back to your old way of life by starting to practice and feel relieved.
How is cervical osteochondrosis treated
Several groups of medicines are prescribed for the basic treatment of medicines.
- Painkillers are prescribed in tablets, or for particularly severe pain, novocaine blockade.
- Nonsteroidal anti-inflammatory drugs - Nurofen, Diclofenac.
- Irritating ointments - finalgon, kapsicam.
- Preparations for relaxation of neck muscles - muscle relaxants.
- A course of intramuscular injections of B vitamins
Support using electricity, massage, warming (insert cans, mustard plaster) is prescribed during the period of relief of the main pain syndrome. During the period of deterioration, the pain always appears, to relieve them, as well as muscle tension, perform the complex of exercise therapy presented above, apply a budget pepper plaster.
Important: any head-turning exercise is prohibited in the case of vertebral artery syndrome, when the vessels of the neck are compressed due to osteochondrosis.
At home, it is effective to make relaxing baths with herbal decoctions, compresses and rubs (for example, using propolis, aloe). The Russian bath copes well with muscle tension. A traditional steam room with a broom relaxes, reduces pain and rejoices.
In extreme cases, it is necessary to direct surgical intervention, when there is a risk that complications due to compression may lead to disability. Namely - complete compression of blood vessels or nerves, significant increase in osteophytes or the appearance of a hernial extension. The operation is performed according to all the rules of neurosurgery - under a microscope and with minimal incisions.





































